PANDORA: Digital Twins and AI for Cardiovascular Surgery

Cardiovascular surgery, particularly operations on the ascending aorta, is among the most delicate procedures in medicine. Aortic aneurysms are one of the most severe cardiovascular conditions: they involve a dangerous dilation of the aorta—the main vessel carrying blood from the heart to the rest of the body—which can eventually rupture with fatal consequences. When they occur in the ascending tract (Figure 1), the portion of the aorta emerging directly from the heart, the risk is especially high, and surgical intervention is the standard of care. In such cases, the diseased segment is replaced with a vascular graft made of Dacron, a synthetic and durable material designed to restore normal blood flow.
The number of these reparative surgeries is expected to grow significantly in the coming years. According to the latest European guidelines, the threshold for surgical treatment has been lowered: while in the past intervention was recommended once the aneurysm diameter exceeded 55 mm, today the critical size has been reduced by 5 mm. Even stricter criteria apply to patients with genetic predispositions, bicuspid aortic valves, or other comorbidities, meaning that more patients will now be eligible for earlier surgical intervention.
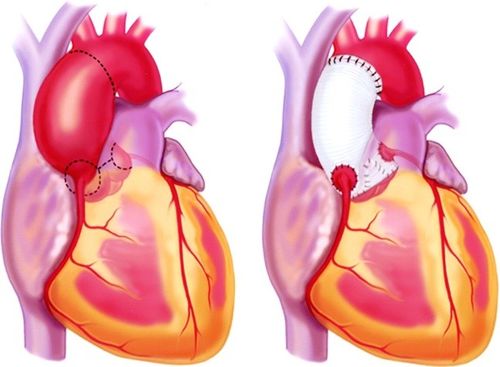
Figure 1: Ascending aortic aneurysm and aortic replacement
Although clinical practice is evolving with more stringent criteria, outcomes remain challenging: around 20% of patients require a secondary surgery within 10 years due to complications or device-related issues. This suggests that, in the near future, we may face a growing pool of patients not only undergoing their first procedure but also requiring re-intervention, adding further pressure on healthcare systems and surgical teams.
Artificial Intelligence (AI) and Digital Twin technologies are now opening the door to a new era of surgical planning. While existing platforms allow clinicians to measure anatomical features from CT or MRI scans, not all can predict how devices will perform once implanted.
This is the gap that the PANDORA project—and its main partner, LivGemini—aims to address in the cardiovascular field.
Within PANDORA, supported by the Italian company RBF Morph SRL, the Signal and Image Processing Laboratory (LTSI) in Rennes, and the National Institute of Applied Sciences of Lyon, LivGemini is developing a software prototype capable of transforming medical images into a patient-specific Digital Twin of the aorta. Using this interactive solution, surgeons will be able to virtually test different vascular grafts and immediately view predictive results on stress distribution, graft deformation, and coronary flow. Behind the scenes, these insights are powered by high-performance computing (HPC) simulations, compressed into surrogate models that deliver answers in near real time. Importantly, all of this occurs within the hospital environment, ensuring patient data remains private and fully compliant with regulations. A first prototype of the software solution is shown in Figure 2.

Figure 2: Prototype of the software solution for replicating the aortic aneurysm surgery.
LivGemini’s expertise in Digital Twin development builds on years of research carried out in previous European projects, most notably MeDiTATe, where several of the researchers now involved in PANDORA were also active. During MeDiTATe, the idea of applying in-silico modelling to cardiovascular surgery emerged, driven by unmet needs expressed directly by surgeons. Since then, the team has consolidated strong expertise in combining numerical simulations, AI-driven models, and clinical workflows. What sets LivGemini apart is its close interaction with the clinical world: the team collaborates daily with surgeons, attends operations, and observes procedures first-hand in order to design solutions that are truly aligned with surgical practice and constraints. This continuous dialogue ensures that the Digital Twin technology developed within PANDORA is not only scientifically advanced but also clinically relevant and directly applicable in real-world settings.
The team is now working on predictive models that can provide surgeons with reliable, patient-specific insights before surgery. Beyond AI-driven segmentation—performed with deep learning architectures such as U-Net to extract accurate 3D reconstructions of the aorta from CT data—the team is developing computational simulations that reproduce the full surgical scenario. These simulations are not limited to the prosthesis itself: they even model the suturing threads used to anchor the vascular graft to the native aorta. This level of detail enables investigation, with unprecedented accuracy, of how the prosthesis adapts to each patient’s anatomy, how local stresses are distributed, and how the graft will perform over time. By integrating these high-fidelity numerical simulations with surrogate modelling techniques, PANDORA aims to deliver fast, clinically interpretable predictions that directly support surgical decision-making.
Such high-fidelity simulations, once integrated into surrogate models, can generate predictions within clinical timeframes. This capability translates into tangible benefits for hospitals: fewer complications, shorter operating times, and reduced need for costly re-interventions. For medical device manufacturers, it opens the possibility of bundling predictive planning software with their devices, strengthening competitiveness and clinical support.
The first application focuses on ascending aortic aneurysms, but the platform has been designed with scalability in mind, allowing future extensions to other cardiovascular interventions such as valve surgery or atrial procedures. This vision is already supported by early collaborations with the University Hospital of Rennes in France and Policlinico Tor Vergata in Italy, which are assisting with the first steps of clinical validation. Through these joint efforts, the combination of AI segmentation, predictive models, and in-silico simulations developed within PANDORA is being translated into a practical tool that enables clinicians to test different options before entering the operating room, reducing uncertainty and improving surgical planning.
Learn more about the PANDORA sub-project here.
The main partner in the project is LivGemini, an Italian innovative start-up and winner of the 2023 Italian Innovation Award in the MedTech sector. The company develops software based on the integration of Digital Twin and Artificial Intelligence to support cardiovascular surgeons in diagnosis and pre-operative planning.
Author: Leonardo Geronzi, Co-Founder & CEO, LivGemini
